Learn about the interesting research findings around Hashimoto’s and gluten, what this could mean for your symptom management, and the steps you should take.
Could a gluten-free diet improve your Hashimoto’s Thyroiditis (HT) if you do not have celiac disease? The answer is it may! Research shows that for those with Hashimoto’s Thyroiditis (HT), a gluten-free diet may decrease health complications and prevent disease progression.
To gain a better understanding of this Hashimoto’s and gluten connection, let’s first start with a closer look at what Hashimoto’s Thyroiditis is.
What Is Hashimoto’s Thyroiditis (HT)?
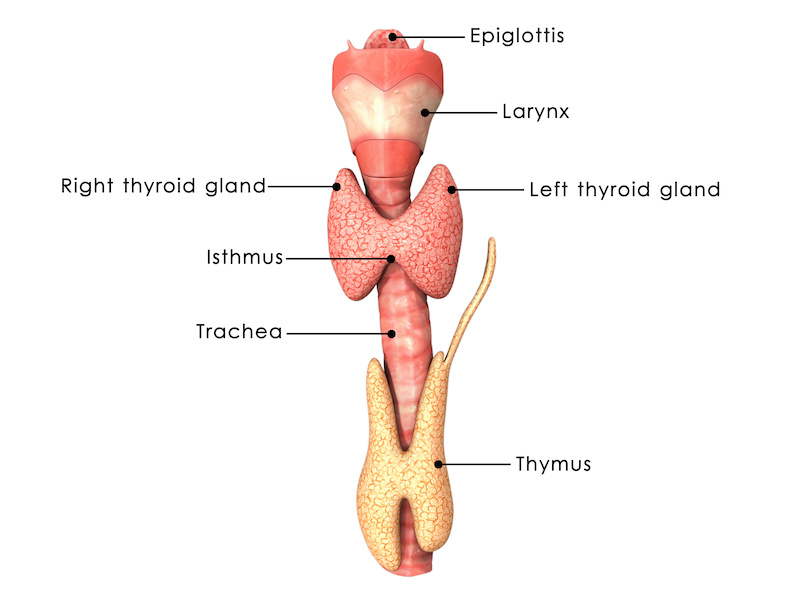
HT is an autoimmune disorder that causes the body’s immune system to attack the thyroid gland and can cause the destruction and scarring of thyroid tissue. (27) The thyroid gland is a butterfly-shaped organ that sits near the base of the neck (between the collar bone and Adam’s apple).
Small, but powerful, the thyroid affects every cell in your body as it produces hormones that regulate:
- metabolism
- heart rate
- breathing
- body temperature
- blood pressure
- the menstrual cycle
Hashimoto’s and Hypothyroidism
With HT, the immune system perceives thyroid cells as harmful and attacks the thyroid with antibodies. This weakens the thyroid’s ability to adequately produce its hormones and can lead to hypothyroidism. (14, 24)
Hypothyroidism occurs when an insufficient amount of thyroid hormones is produced, resulting in many health complications. Although the standard treatment is to take thyroid replacement therapy (levothyroxine), many people find it difficult to stabilize their disease, resulting in continued health consequences. (14, 24)
What Causes Hashimoto’s?
The exact cause of Hashimoto’s is unknown, but the interplay among several factors is considered to play roles in affecting thyroid function. These include:
- genetic susceptibility (1,24)
- stress (1,11,12, 24, 27)
- infection (Epstein-Barr virus, hepatitis c) (12, 24)
- nutritional deficiencies such as vitamin d and selenium (1,13, 17, 24, 27) and zinc and magnesium (27)
- insufficient or excess iodine (27)
- environmental factors (including radiation, pesticides, heavy metals, and endocrine disruptors like BPA) (1,12, 17, 23, 25, 27)
- an imbalance of gut microbes (17, 20, 28)
While these are all thought to contribute, the mechanisms are not fully known.
Other Autoimmune Diseases and Hashimoto’s
People with HT may also experience, or be at risk for, other autoimmune diseases like celiac disease which can be diagnosed with markers in the blood and confirmed from intestinal biopsies. (26) Intestinal biopsies of some HT patients may even show signs of “potential celiac disease”. (8) The two diseases share many similarities and dissimilarities. (17)
Hashimoto’s Diet
Navigating a nutritional approach to HT management can be challenging. Many people with HT may be lactose intolerant. (27) In addition to gluten, there may be other foods that can cause the immune system to attack thyroid tissue. (27)
Untreated hypothyroidism can lead to high cholesterol and constipation. (4) Minimizing dietary cholesterol and increasing water and fiber intake can help. Foods such as grapefruit juice, espresso coffee, and soy, particularly those containing iron and calcium can affect the absorption of levothyroxine when taken together. (4)
A deficiency of minerals such as iodine, iron, zinc, selenium, copper and magnesium, vitamins A, C, D, and B groups, as well as omega-3 fatty acids are also not uncommon in people with HT. (27) Eating foods containing these nutrients and those rich in antioxidants is essential for proper thyroid and immune function. (27)
Some people mistakenly consume high doses of iodine, thinking it will enhance the thyroid’s ability to produce hormones (iodine is needed to produce thyroid hormones). Unfortunately, excess iodine often has the exact opposite effect on people with HT, causing even more antithyroid antibodies to be produced and a worsening of hypothyroid symptoms. (1,4,17, 24) That happened to me and my son.
What Is Gluten?
Gluten is a complex mixture of proteins. It accounts for approximately 80% of the total protein in wheat and is also present in rye and barley. (7, 19, 22)
- It can be found in the starchy endosperm of these grains. Although the composition and distribution of gluten proteins differ among wheat varieties, the main proteins in wheat are known as gliadin and glutelin. (7, 22)
- Gluten acts as a binder and gives food a stretchy quality. Think of tossing a pizza dough and watching it expand. In addition to wheat, rye, and barley, gluten can be found in many foods.
- Learn more about gluten-free diets by reading

What The Research Says About Hashimoto’s and a Gluten-Free Diet
Studies have shown that a gluten-free diet may lower antithyroid antibodies and improve absorption of levothyroxine in those with both celiac disease and HT. (7, 9, 17) However, in non-celiac patients with HT, there is a lack of research on how a gluten-free diet affects antithyroid antibodies. (7, 17,27)
Recent Research about Hashimoto’s and Gluten
Fortunately, a few studies give some direction:
- In women with HT, celiac disease blood markers, and an absence of celiac disease symptoms, six months of a gluten-free diet was shown to lower antithyroid antibodies. Vitamin D levels unexpectedly increased. The authors concluded that the strict gluten-free diet may have directly inhibited attacks on the thyroid and improved its function. (10)
- In women with HT who adhered to a gluten-free diet and were given supplemental selenium, antithyroid antibody levels were significantly reduced. Thyroid function and autoimmunity improved after six months. (17, 18)
- In a case study of a 23-year-old female, a gluten and grain-free diet in combination with stress management and supplementation of selenium, zinc, antioxidants, and other nutrients improved gut microbiota and reduced thyroid antibodies. (31)
The Gut Thyroid Connection – The Gut and Hashimoto’s
Increased intestinal permeability (often referred to as leaky gut) is linked with interrupting the immune system’s ability to properly function (3, 19) Not surprisingly, those with HT may have intestinal permeability and be at greater risk for developing intestinal bacterial overgrowth. (27)
With increased permeability and inflammation, gluten can enter the bloodstream and portions of it can be altered by enzymes into a structure that appears harmful to the immune system. Unfortunately, this new structure may mimic tissue found in the thyroid gland setting the ground for the immune system to attack the thyroid. (14, 16)
Leaky Gut
Here’s how a leaky gut may emerge.
- Zonulin, a protein produced in our intestines and liver, mediates the permeability of our gut lining. (3)
- Gluten, large amounts of bacterial overgrowth, and/or changes in bacterial composition can trigger the production of zonulin.
- Because our body cannot completely digest gluten, the more undigested gluten present, the higher the zonulin levels produced and the more permeable our gut lining becomes. (3, 7)
Elevated levels of zonulin have been found in individuals with autoimmune diseases. (7) In a pilot study, children with HT were found to have higher levels of zonulin than those children with congenital hypothyroidism indicating increased intestinal permeability. (2)
In a study evaluating the gut bacteria of HT adults, researchers found increased intestinal permeability from higher concentrations of zonulin in the blood compared to adults without HT (29) The diversity and richness of bacteria in the gut of HT adults were also found to be low (29, 30). Interestingly, increased intestinal permeability precedes several autoimmune disorders. (2)
Can Going Gluten-Free Improve Your Autoimmune Symptoms and Lower Your Antithyroid Antibodies?
Anecdotally, it did for me and my son. We do not have celiac disease. Yet, as with non-celiac gluten sensitivity people, a gluten-free diet improved our digestion and overall health. Individuals undiagnosed with either celiac disease or wheat allergies who report improved intestinal symptoms (e.g. irritable bowel syndrome) and/or extra-intestinal symptoms from a gluten-free diet are said to have non-celiac gluten sensitivity (NCGS). (5) According to the Celiac Disease Center at Columbia University, there are no specific tests validated to diagnose NCGS at this time.
Anecdotal Evidence on Gluten-Free in Private Practice
Although there is a lack of agreement about whether NCGS correlates with increased intestinal permeability or whether it activates the immune system (6), there is a high prevalence of autoimmune thyroid disease in people experiencing NCGS (7).
Studies may be limited, but certain autoimmune diseases have responded to a gluten-free diet. (19,21) Some practitioners have seen positive effects of a gluten-free diet for their patients with autoimmune conditions like HT, lupus, fibromyalgia, and rheumatoid arthritis. After years of trying to regulate our HT, both my adult son and I witnessed a reduction in our antithyroid antibodies after we switched to a healthy, nutrient-dense gluten-free diet.
Next Steps to Take with Hashimoto’s and Gluten In Mind
Although there is no known cure for HT, studies provide a strong incentive to maintain a healthy, balanced gut microbiota and a low inflammatory diet. (27,29) Here are some steps you can take for a balanced diet:
- Meet with a registered dietitian to evaluate if a gluten-free diet is right for you and help identify micronutrient deficiencies.
- Focus on a variety of whole, nutrient-dense foods, free of gluten.
- If you’re following a gluten-free diet, and unsure if your favorite product is indeed free of gluten, gluten detection kits are available to use in or outside the home, one of which was recently assessed by adolescents and adults with celiac disease. (15)
Removing gluten from your diet may decrease the severity of an autoimmune response to undigested gluten crossing into the bloodstream due to inflammation and increased permeability in the intestine. Digestion issues related to intestinal permeability or decreased gastric acid secretion can impact the absorption of nutrients as well as thyroid medication. (14,28) And of course, if you are taking levothyroxine, confirm with the manufacturer that it is free of gluten.
Concerned you may have a gluten-free intolerance or Celiac, book an appointment for nutrition counseling today!
References
- Ajjan RA, Weetman AP. The Pathogenesis of Hashimoto’s Thyroiditis: Further Developments in our Understanding. Horm Metab Res. 2015;47(10): 702-710. Doi: 10.1055/s-0035-1548832
- Aydin BK, Yildiz M, Akgun A, et al. Children with Hashimoto’s Thyroiditis Have Increased Intestinal Permeability: Results of a Pilot Study. J Clin Res Pediatr Endocrinol. 2020;12(3): 303-307. Doi: 10.4274/jcrpe.galenos.2020.2019.0186
- Fasano A. F1000Res. [Published online] 2020 A disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. Doi. 10.12688/f1000research.20510.1
- National Institute of Diabetes and Digestive and Kidney Diseases [Updated 2021 June]. Hashimoto’s Disease. (page 6, paragraph 4). https://www.niddk.nih.gove/health-information/endocrine-diseases/hashimotos-disease#common.
- Leonard MM, Sapone A, Catassi C, et al. Celiac disease and nonceliac gluten sensitivity: a review. JAMA. 2017;318(7): 647-656. Doi: 10.1001/jama.2017.9730
- Catassi C, Alaedini A, Bojarski C, et al. Overlapping Area of Non-Celiac Gluten Sensitivity (NCGS) and Wheat-Sensitive Irritable Bowel Syndrome (IBS): An Update. Nutrients. 2017;9(11): 1268. Doi: 10.3390/nu9111268
- Passali M, Josefsen K, Frederiksen JL, et al. Current Evidence on the Efficacy of Gluten-Free Diets in Multiple Sclerosis, Psoriasis, Type 1 Diabetes and Autoimmune Thyroid Diseases. Nutrients. 2020; 12:2316. Doi: 10.3390/nu12082316
- Valentino R, Savastano S, Maglio M, et al. Markers of potential coeliac disease in patients with Hashimoto’s thyroiditis. Eur J Endocrinol. 2002;146(4): 479-483. Doi: 10.1530/eje.0.1460479
- Sategna-Guidetta C, Volta U, Ciacci C, et al. Prevalence of thyroid disorders in untreated adult celiac disease patients and effect of gluten withdrawal: An Italian multicenter study. Am J Gastroenterol. 2001;96(3): 751-757. Doi: 10.1111/j.1572-0241.2001.03617.x
- Krysiak R, Szkrobka W, Okopien B. The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp Clin Endocrinol Diabetes. 2019; 127(7):417-422. Doi: 10.1055/a-0653-7108
- Markomanolaki ZS, Tigani X, Siamatras T, et al. Stress Management in Women with Hashimoto’s Thyroiditis: A Randomized Controlled Trial. J Mol Biochem. 2019;8(1): 3-12.
- Dittfeld A, Gwizdek K, Michalski M, et al. A possible link between the Epstein-Barr virus infection and autoimmune thyroid disorders. Cent Eur J Immunol. 2016;41(3): 297-301. Doi: 10.5114/ceji.2016.63130.
- Liontiris MI, Mazoopakis EE. A Concise review of Hashimoto thyroiditis (HT) and the importance of iodine, selenium, vitamin D an gluten on the autoimmunity and dietary management of HT patients. Points that need more investigation. Hell J Nucl Med. 2017;20(1):51-56. Doi: 10.1967/s002449910507
- Mincer DL, Jialal I. Hashimoto Thyroiditis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 28, 2021
- Wolf RL, Vipperman-Cohen A, Green PHR, et al. Portable gluten sensors: qualitative assessments by adults and adolescents with coeliac disease. J Hum Nutr Diet. 2020;33(6): 876-880. Doi: 10.111/jkn.12810
- Vojdani A, Tarash I. Cross-Reaction between Gliadin and Different Food and Tissue Antigens. Food Nutr Sci. 2013;3: 20-32. Doi: 10.4236/fns.2013.41005
- Ihnatowicz P, Wator P, Drywien ME. The importance of gluten exclusion in the management of Hashimoto’s thyroiditis. Ann Agric Environ Med. 2021;28(4): 558-568. Doi: 10.26444/aaem/136523
- Asimi AV, Hadzovic-Dzuvo A, Tawil DA. The effect of selenium supplementation and gluten-free diet in patients with subclinical hypothyroidism affected by autoimmune thyroiditis. Endocrine Abstracts. 2020;70: AEP906. Doi: 10.1530/endoabs.70.AEP906
- Lerner A, Shoenfeld Y, Matthias T. Adverse effects of gluten ingestion and advantages of gluten withdrawal in nonceliac autoimmune disease. Nutr Rev. 2017;75:1046-1058
- Mori K, Nakagaqa Y, Ozaki H. Does the gut microbiota trigger Hashimoto’s thyroiditis? Discov Med. 2012;14(78): 321-326.
- Lerner A, Ramesh A, Torsten M. Going gluten free in non-celiac autoimmune diseases: the missing ingredient. Expert Rev Clin Immunol. 2018;14(11): 873-875. Doi: 10.1080/1744666x.2018.1524757
- Biesiekierski J. What is gluten? J Gastroenterol Hepatol. 2017;32(S1): 78-81. Doi: 10.1111/jgh.13703
- Kim MJ, Park YJ. Bisphenols and Thyroid Hormone. Endocrinol Metab (Seoul). 2019;34(4):340-348. Doi:10.3803/EnM.2019.34.4.340
- Ragusa F, Fallahi P, Elia G, et al. Hashimotos’ Thyroiditis: Epidemiology, pathogenesis, clinic and therapy. Best Pract Res Clin Endocrinol Metab. 2019;33(6). Doi: 10.1016/j.beem.2019.101367
- Kahn LG, Liu X, Rajovic B, et al. Blood lead concentration and thyroid function during pregnancy: results from the Yugoslavia Prospective Study of Environmental Lead Exposure. Environ Health Perspect. 2014;122(10):1134-1140. Doi:10.1289/ehp.1307669
- Ch’ng CL, Jones MK, Kingham JG. Celiac disease and autoimmune thyroid disease. Clin Med Res. 2007;5(3):184-192. Doi:10.3121/cmr.2007.738
- Ihnatowicz P, Drywień M, Wątor P, Wojsiat J. The importance of nutritional factors and dietary management of Hashimoto’s thyroiditis. Ann Agric Environ Med. 2020;27(2):184-193. Doi:10.26444/aaem/112331
- Fröhlich E, Wahl R. Microbiota and Thyroid Interaction in Health and Disease. Trends Endocrinol Metab. 2019;30(8):479-490. Doi:10.1016/j.tem.2019.05.008
- Cayres LCF, de Salis LVV, Rodrigues GSP, et al. Detection of Alterations in the Gut Microbiota and Intestinal Permeability in Patients With Hashimoto Thyroiditis. Front Immunol. 2021;12:579140. Doi:10.3389/fimmu.2021.579140
- Liu S, An Y, Cao B, Sun R, Ke J, Zhao D. The Composition of Gut Microbiota in Patients Bearing Hashimoto’s Thyroiditis with Euthyroidism and Hypothyroidism. Int J Endocrinol. 2020;2020:5036959. Doi:10.1155/2020/5036959
- Avard N, Grant SJ. A case report of a novel, integrative approach to Hashimoto’s thyroiditis with unexpected results. Adv Integr Med. 2018;5(2): 75-79. Doi:10.1016/j.aimed.2018.03.003